Thoracic aortic aneurysm surgery becomes necessary when the aneurysm reaches a certain size or exhibits rapid growth, posing an increased risk of rupture or dissection. The decision for surgical intervention is primarily based on the aneurysm's size and location, as well as the patient's overall health and medical history.
What is a Thoracic Aortic Aneurysm?
A thoracic aortic aneurysm is a potentially life-threatening condition characterized by an abnormal bulging or ballooning of the aorta in the chest area. The aorta is the main artery that carries oxygenated blood from the heart to the rest of the body. When an aneurysm develops, the weakened section of the aortic wall expands, making it susceptible to rupture or dissection. This condition can be caused by various factors, including age, high blood pressure, atherosclerosis (build-up of fatty deposits in the arteries), genetic disorders, and connective tissue diseases like Marfan syndrome or Ehlers-Danlos syndrome. Thoracic aortic aneurysms are often asymptomatic in their early stages, making regular health check-ups and screening vital for early detection and intervention.
The management of thoracic aortic aneurysms depends on their size, location, and the risk of rupture. Smaller aneurysms may be closely monitored through regular imaging tests, while larger or rapidly growing aneurysms may require surgical intervention. Timely diagnosis and appropriate treatment are essential to prevent complications and improve patient outcomes. Patients diagnosed with thoracic aortic aneurysms are often advised to adopt heart-healthy lifestyle changes, such as managing blood pressure, maintaining a balanced diet, quitting smoking, and engaging in regular physical activity to reduce the risk of aneurysm growth and rupture.
The Importance of Early Detection
Early detection of thoracic aortic aneurysm is crucial for ensuring timely and effective surgical intervention. Detecting an aneurysm at an early stage allows medical professionals to closely monitor its size and progression, enabling them to make informed decisions regarding the appropriate timing for surgery. Surgical repair of thoracic aortic aneurysms is often recommended when the aneurysm reaches a certain size or shows rapid growth, as larger aneurysms are at a higher risk of rupture, which can be life-threatening.
By undergoing thoracic aortic aneurysm surgery early, patients can significantly reduce the risk of complications and potentially life-threatening events. Surgical repair involves reinforcing the weakened section of the aorta, preventing further expansion and reducing the risk of rupture or dissection. Moreover, early intervention can also lead to better surgical outcomes and shorter recovery periods for patients, allowing them to resume their normal activities sooner and improve their overall quality of life.
Regular health check-ups and screenings are essential for early detection, especially for individuals with risk factors such as a family history of aortic aneurysms, connective tissue disorders, or a history of smoking or hypertension. By being proactive about their heart health and seeking medical attention if any symptoms or risk factors are present, individuals can ensure early detection of thoracic aortic aneurysms, paving the way for timely surgical intervention and ultimately better health outcomes.
When is Surgery Necessary?
Generally, surgical repair is recommended for thoracic aortic aneurysms that are larger than 5.5 centimeters in diameter, as these aneurysms have a higher risk of rupture. Additionally, surgery may be considered for aneurysms that show rapid expansion, regardless of their size, to prevent potential complications.
In some cases, the surgical decision may be influenced by the presence of symptoms or the aneurysm's location. If the aneurysm is causing pressure on surrounding organs or structures, leading to symptoms such as chest pain, difficulty swallowing, or breathing problems, surgery may be advised to relieve the pressure and improve the patient's quality of life.
Ultimately, the decision for thoracic aortic aneurysm surgery is made by a team of experienced cardiac surgeons and specialists, who carefully assess the individual's condition and risks. They take into consideration factors such as the aneurysm's size, growth rate, location, the patient's age, overall health, and any other relevant medical conditions. Early intervention with surgery can help prevent life-threatening complications and improve patient outcomes, making it essential to closely monitor thoracic aortic aneurysms and consider surgery when appropriate.
Risks and Complications in Thoracic Aortic Surgery
Thoracic aortic aneurysm surgery, like any major surgical procedure, carries certain risks and potential complications. It is essential for patients to be aware of these risks and for medical teams to take necessary precautions to minimize them.
Some of the common risks and complications associated with thoracic aortic aneurysm surgery include:
- Bleeding: During surgery, there is a risk of excessive bleeding, which can be managed with proper surgical techniques and blood transfusions if necessary.
- Infection: Surgical sites are susceptible to infections, but preventive measures, such as antibiotic administration, are taken to minimize this risk.
- Blood Clots: Formation of blood clots in the legs or lungs (deep vein thrombosis or pulmonary embolism) can occur after surgery. Patients are encouraged to move and walk as soon as possible to prevent this complication.
- Anesthesia Risks: Anesthesia can lead to adverse reactions, although modern anesthetic techniques have significantly reduced such risks.
- Organ Damage: There is a possibility of injury to nearby organs during surgery, though skilled surgeons take precautionary measures to avoid this.
- Stroke: In some cases, there is a risk of stroke during or after surgery due to emboli or reduced blood flow to the brain.
- Spinal Cord Injury: For surgeries involving the descending aorta, there is a rare risk of spinal cord injury, which can lead to paralysis or weakness in the legs.
- Aortic Valve Dysfunction: Surgery may affect the functioning of the aortic valve, leading to valve-related complications.
- Endo-leak: In endovascular repair procedures, a persistent flow of blood within the aneurysm (endo-leak) may occur, necessitating further intervention.
Despite these potential risks, thoracic aortic aneurysm surgeries are generally considered safe and highly successful when performed by experienced cardiac surgical teams. Surgeons carefully evaluate each patient's medical history and overall health to make informed decisions and minimize the risks associated with the procedure. Patients are encouraged to discuss any concerns or questions they may have about the surgery with their healthcare providers to ensure they have a clear understanding of the potential risks and benefits.
Decision Making
The decision on how to best treat a thoracic aortic aneurysm or the aorta depends on its size and rate of its growth, location and your overall health. The risk of rupture increases when the aneurysm is larger than about twice the normal diameter of a healthy aorta blood vessel.
If a thoracic aneurysm is small and causes no symptoms, your physician may recommend “watchful waiting,” which includes:
- Close monitoring of the aneurysm with CT or MRI scans every 6 months.
- Blood pressure medication to control high blood pressure, and decrease pressure on the weakened area of the aneurysm.
- Restriction of some physical activities. Heavy lifting should be avoided as increased pressure on the aorta, may put an aneurysm at risk of rupture.
Thoracic Aortic Aneurysm Surgery Decision Making
The decision to treat a thoracic aneurysm with surgery is determined by many factors, including:
- If the symptoms include chest, back pain, pain in the jaw, neck and upper back.
- If the aneurysm is growing more than 1 (cm) centimeter per year.
- Signs of an aortic dissection, including sudden, severe sharp tearing pain in the chest or back.
- The age of the patient and the patient’s overall medical condition.
New evidence has shown that the size of the aneurysm in addition to a patient’s height plays an important role in the decision for surgery. While 5 centimeters is the size most aneurysms are considered for surgery, Cleveland Clinic surgeons have compiled years of experience and published studies to find that a patient’s height and their aneurysm’s size strongly correlates with the need for surgery.
Due to highly individualized characteristics guiding the decision for surgery, it is best that a physician regularly monitors patient’s thoracic aneurysm.
How Is Thoracic Surgery Treated?
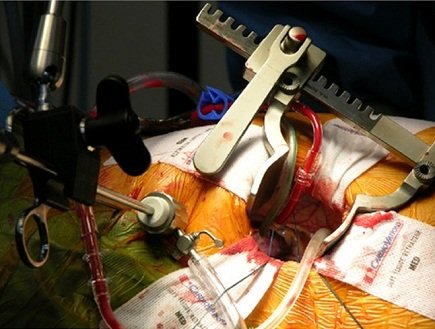
The current standard surgical treatment of a thoracic aortic aneurysm is the open-chest approach. The main purpose of open-chest surgery to treat a thoracic aneurysm is to replace the weakened portion of the aorta with a fabric tube, called a graft.
Repairing a thoracic aneurysm is surgically complicated and requires an experienced thoracic surgical team. However, neglecting the aneurysm presents a higher risk.
At Fortis Escorts Heart Institute, we have a dedicated team lead by Dr. Ritwick Raj Bhuyan who has performed these procedures with results similar to international standards.




