Endocarditis Surgery
Endocarditis is the infection that affects the heart valves or any structure within it (valve prostheses, pacemaker cables or defibrillators, and other catheters).
Each year, 3-4 new cases are detected per 100,000 inhabitants. Their frequency increases with age so that in individuals aged 70-80 the incidence reaches 15 cases per 100,000 inhabitants.
Endocarditis is usually classified into four groups, which differ by their clinical picture, their treatment, and their prognosis:
- Endocarditis on the native valve (the patient’s normal valve).
- Endocarditis on the prosthetic valve (a prosthesis previously implanted).
- Implantable pacemaker and defibrillator endocarditis.
- Endocarditis in injecting drug users (intravenous).
The bacteria are responsible for the infection and, less frequently, fungi. Streptococci, enterococci, and staphylococci are among the most common bacteria, but almost any bacteria can cause endocarditis. Knowing the germ that causes the infection is of vital importance for the treatment of the disease.
The most common symptom of endocarditis is fever (usually equal to or greater than 38 degrees). Usually accompanied by shivering. It is usual for patients to have other non-specific symptoms or that may lead us to believe that this is another disease, such as neurological, cardiologic, pulmonary, renal, abdominal, rheumatic, etc.
Often patients in addition to fever present with analytical alterations, a new heart murmur and/or embolisms. Weight loss, lethargy, enlarged spleen, and abscesses on the skin, brain, liver, or lungs may also occur.
In principle, any individual can suffer endocarditis. However, there are a number of patients at greater risk of suffering from the disease, although each group of those listed below does not have the same risk of suffering from it:
- The carriers of a valvular prosthesis and/or any intracardiac device.
- Patients with rheumatic valve disease (mitral stenosis, mitral insufficiency, aortic insufficiency), degenerative (elderly, renal patients) or others (mitral valve prolapse with mitral insufficiency).
- Patients with obstructive hypertrophic cardiomyopathy.
- Patients who have already had an episode of endocarditis.
- Patients with certain congenital heart defects.
- Those who have undergone a heart transplant and have developed a new valve disease.
Medical Treatment of Endocarditis
This disease is usually treated by combining two or three antibiotics intravenously at high doses. The treatment time lasts between four and six weeks. The most commonly used antibiotics are penicillin, cloxacillin, vancomycin, gentamicin, rifampicin, ampicillin, and ceftriaxone.
When infective endocarditis is suspected, the extraction of several blood cultures (blood culture) is essential to know the germ that causes the infection and to be able to use the specific antibiotics against it. Until the microorganism is known, predefined patterns are used depending on the type of endocarditis (on the valve, prosthetic, intracardiac devices, or in patients who use injecting drugs) and whether it occurs in an acute or chronic way.
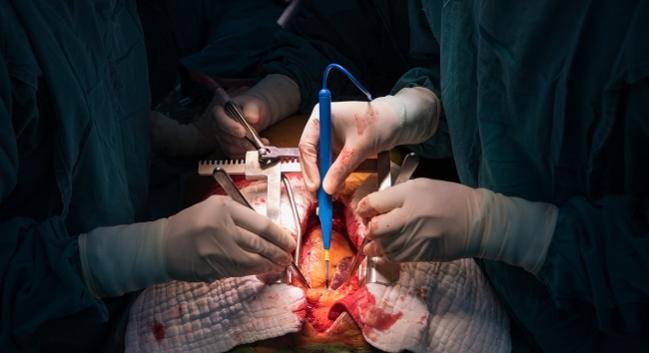
Surgical Treatment of Endocarditis
Although antibiotic treatment is effective in many patients, up to 50% will need to undergo surgery. In these cases, it will be necessary to replace the valve infected by a prosthesis in addition to the antibiotic treatment, to obtain a definitive treatment of the disease.
There are three classic indications for early (short-term) surgery in infective endocarditis:
- The appearance of heart failure (more frequent and severe complication).
- The presence of uncontrolled infection, which is defined as the persistence of fever and positive blood cultures despite the appropriate antibiotic treatment for the germ that produces it.
- The appearance of new embolisms despite adequate antibiotic treatment.
The surgery, which in these cases is usually urgent, will be directed in all cases to restore valvular function. It is performed with extracorporeal circulation and technically not much different from a conventional cardiac surgery (see sections: During Cardiac Surgery and Mitral Valve Repair ), except for the peculiarity that the main goal is the complete removal of infected tissue. To do this, complex reconstructions of cardiac structures sometimes have to be performed. They should be debrided, ie cleaned of necrotic tissue and diseased aspect, abscessed areas if they exist.
In most cases, the valve (s) affected by a prosthesis will be replaced. In some cases, implantation of a pacemaker may be necessary if the infection has affected the electrical conduction tissue of the heart.
In spite of the surgical treatment, it is essential to continue in the postoperative period with the appropriate antibiotic treatment, which is usually prolonged several weeks after the surgery.
Prophylaxis and Prevention of Endocarditis
From a general point of view, it is fundamental to follow a series of norms that, although they are applicable to the general population, must be more rigorously fulfilled in the patients at risk of endocarditis:
- Mouth care and proper oral hygiene.
- Skincare (to avoid injuries and infections).
- Asepsis in the operating room and post-operative care units (source of precocious prosthetic endocarditis), in order to avoid intravenous infection, which is a frequent source of infection in hospitalized patients. Urinary tract catheterization should also be limited to cases where it is necessary and kept as short as possible.
- Extreme cleaning in patients who undergo dialysis, as well as in the implantation of pacemakers and defibrillators.
Prophylaxis of endocarditis involves the administration of a single dose of antibiotics prior to the performance of certain procedures that can cause a spread of bacteria into the bloodstream. This must be done in those subjects with a higher risk of acquiring the disease; Mainly patients with a valvular prosthesis, patients who have suffered prior endocarditis, patients with complex congenital heart disease and patients with previous heart transplantation who also suffer from valvular disease.




